Just as we thought India’s COVID-19 second wave is plateauing in most states, mucormycosis or black fungus infection cases began to rise rapidly. The rising number of cases of this fungal infection took the healthcare infrastructure and administration by surprise and has now been declared an epidemic by the government. India has 71% of the total mucormycosis cases reported in the world.
What is the Black Fungus Infection?
Black fungus infection, also called mucormycosis, is caused by mucormycetes, a type of fungus. It is a rare, deadly, non-contagious fungal infection and can prove fatal if not treated promptly. One can get infected with this fungus if they inhale the spores or come in contact with them in soil and decaying matter.

Once an individual is infected, the fungus proliferates in their blood vessels, cutting off blood supply to the tissues and creating its own decaying food source.
Is Mucormycosis Contagious?
Mucormycosis or black fungus infection is not contagious. This means it cannot spread from an infected person to another person or animal. One can get infected by this fungal infection when they come in direct contact with the spores of the fungus or inhale them.
Who is at Risk of Getting the Black Fungus Infection?
The rise of this deadly fungal infection has been observed in recovering COVID-19 patients. What is the link between the two? Well, black fungus infection occurs more commonly in individuals with debilitating diseases and deficient immune systems.
Common risk factors/causes for black fungus infection include:
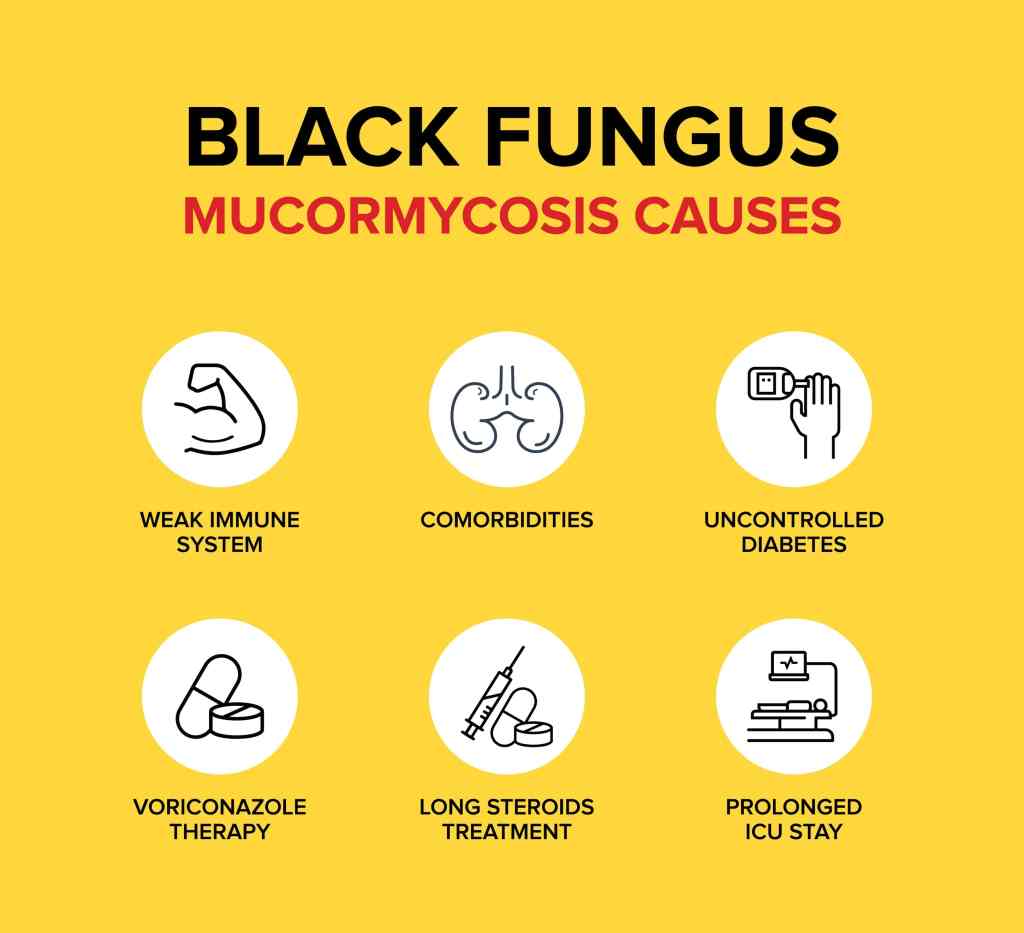
- Diabetes (especially uncontrolled diabetes)
- Long-term use of steroids
- Patients undergoing cancer treatment
- A weak or compromised immune system
- Prolonged stay in the ICU (common in severe COVID-19 cases)
- Excessive iron in the body
- In people who are recovering from surgery, burns, or injuries
Patients whose immune systems have been compromised due to illnesses like the COVID-19 disease find it difficult to ward off infections like mucormycosis. It has also been suspected that COVID-19 patients on prolonged oxygen support are at an increased risk of developing the black fungus infections due to unclean or contaminated water used to supply the oxygen.
What are the Symptoms of Black Fungus?
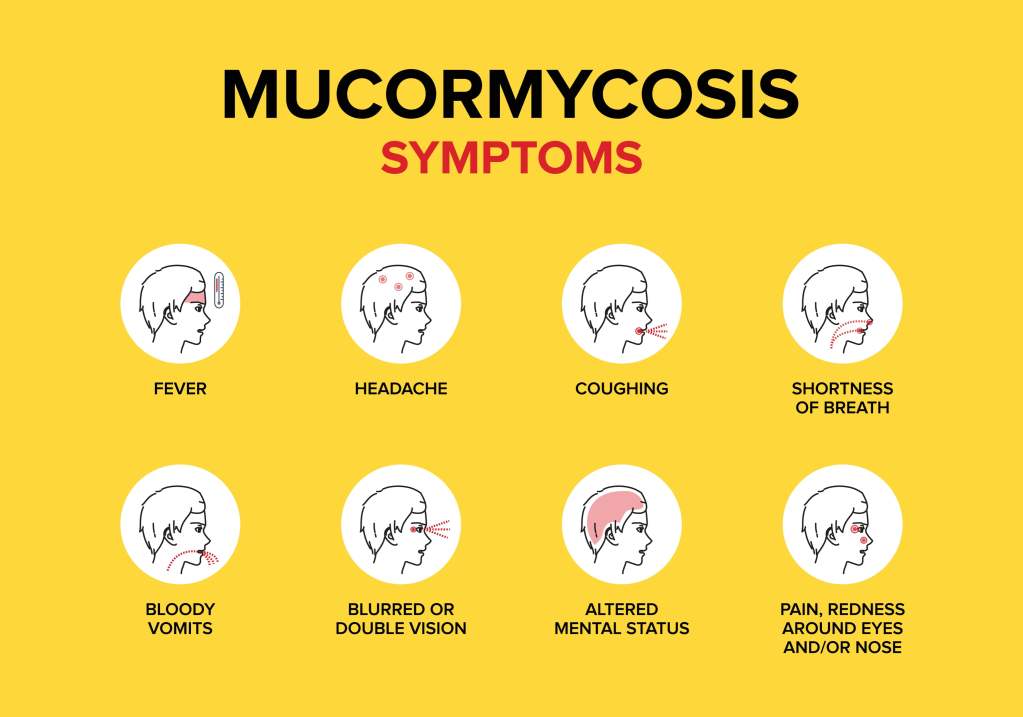
The key to successfully treating black fungus infections is early detection and prompt treatment. The symptoms of mucormycosis depend upon the area of the body the fungus affects.
Black fungus symptoms include:
- Black coloured crusting or scabbing around the nose
- Fever
- Headache
- Reddish swelling around the nose and sinuses
- Unilateral facial swelling
- Nasal or sinus congestions
- Delirium
- Memory loss
- Blurry or double vision
When mucormycosis affects the lungs, the symptoms vary from those above and include:
- Coughing (which can sometimes produce dark fluid)
- Chest pain
- Shortness of breath
Black fungus symptoms in the gastrointestinal tract include pain in the abdomen, nausea, vomiting, and bleeding.
Disseminated mucormycosis is a condition that can occur in people already suffering from other medical conditions and can have diffused symptoms, making it difficult to spot the condition due to overlapping symptoms.
How is a Black Fungus Infection Treated?
Black fungus infection is usually diagnosed based on the patient’s medical history, symptoms, and history of hospitalisation. A team of professionals, including specialists, surgeons, and microbiologists, are required to treat black fungus infections.
The treatment for mucormycosis needs to begin immediately to stop the fungus spread, owing to the aggressive nature of the disease. The treatment of this disease includes medical and surgical measures based on the spread and severity of the infection in the individual.
Prescription medications used to treat black fungus infection include Amphotericin B, posaconazole, or isavuconazole, which may be given intravenously (through a vein) or orally (by mouth). Along with medications, surgical debridement is performed on the infected area to remove the damaged and infected tissue.
Apart from these treatment measures performed on a war footing, the patient’s underlying conditions like uncontrolled blood sugar levels are brought under control. Steroids are immediately discontinued in patients undergoing steroid therapy.
Long-term fungal medications may be advised to the patient to help in the complete resolution of the black fungus infection.
What are the Complications of the Black Fungus Infection?
If not treated in time, the black fungus infection can lead to severe complications such as:
- Blindness
- Bone infection
- Meningitis
- Abscess in the brain
- Haemorrhages in the lungs or the gastrointestinal tract
- Sepsis
How to Protect Yourself From the Black Fungus Infection?
Many people today are fearing the black fungus infection and wish to prevent it. It is almost impossible to avoid breathing in air that may contain the spores of this fungus. Without a preventive vaccine, preventing mucormycosis may seem like a challenge.
Here are some ways by which you can protect yourself from this black fungus infection:
Avoid areas that can be a breathing ground for this black fungus, such as excavation sites, water-damaged buildings, etc.
If you have to touch the soil, for example, during gardening or other such activities, ensure you have a proper mask, gloves, appropriate shoes, and long pants to avoid coming in direct contact with the spores of the fungus.
If you fall in the high-risk group, your healthcare provider will prescribe medications to prevent fungal infections. This is particularly true for people who have had transplants.
Change the water in the oxygen support regularly to avoid the development of fungus.
Change your mask frequently, preferably after every use. The moist environment is a good breeding ground for the black fungus.
The black fungus infection, commonly seen in patients recovering from a COVID-19 infection, is an aggressive yet rare fungal infection that can cause severe internal damage. Identifying the symptoms and administering immediate treatment can have better treatment outcomes in patients. Leaving this condition untreated can prove to be fatal.
If you wish to help a patient fund their treatment during these critical times, do your bit! Donate to a noble cause on Ketto and help save a life!
Author
Dr. Meenakshi Maruwada
BDS (Nair Hospital Dental College, Mumbai), PGCAD (Mumbai)
GMHE (IIM Bangalore)
https://www.linkedin.com/in/drmeenakshim
- What is Black Fungus, and How Does it Affect Humans? - May 26, 2021
Need Funds for Medical Treatment?
Start a Fundraiser on Ketto and raise the amount for your treatment

